Tick Talk
Understanding Tick Bites and How to Prevent Them
The CritiCare team talked about bee sting protection measures in our earlier blog post. When the weather gets warmer, we need to be aware of more insects than only bees. This weather will also bring out ticks, as they are most common during the warmer months. According to the US Department of Agriculture, Ticks are most active in the months of April-September. This post will review prevention and treatment techniques our caregivers can practice as we approach the summer months.
One of the biggest preventative measure nurses and direct care staff can take during this season, is being mindful of places ticks will be. According to The Center of Disease Control and Prevention, ticks live in grassy, bushy, and wooded areas. When accompanying a patient outside, caregivers should make every effort to stay away from these places. It is best to stay on the designated trail and never venture into the woods whether hiking or taking a walk. As we start assigning PCAs and Nurses on field trips to state parks, summer camps, and other outdoor settings, it is crucial to keep this in mind.
After you come indoors, the CDC emphasizes the importance of following these tips:
- Check clothing for ticks: Our direct care staff members are encouraged to check their clothing and patients, to remove any signs of insects that could potentially be brought inside.
- Shower shortly after being outdoors: The CDC recommends taking a shower after you are at an outdoor activity and doing a body check for any signs of ticks. Our Caregivers are encouraged to educate their patients about this tip as well so they can do this when they go home. Places to check for ticks include:
- Under the arms
- In and round the ears
- Inside the belly button
- Back of the knees
- In and around your scalp
- Around the waist
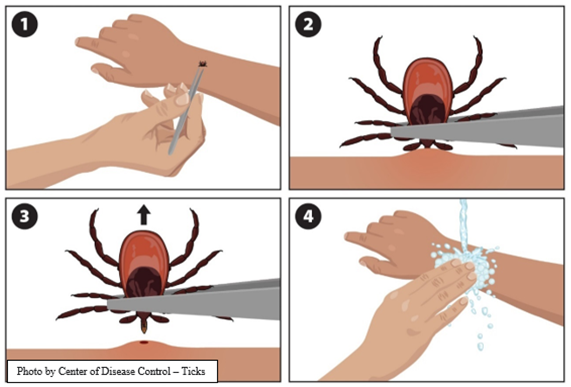
If an employee, patient or client is bitten by a tick, please call to discuss further treatment with their doctor. If a tick has landed on skin, it is important to remove it as soon as possible. The CDC reports that any tweezer is fine to remove a tick from skin.
Step 1: Use tweezers to grab the tick as close to the skin as possible.
Step 2: Once you have the tick, pull upward. Do not twist the tick.
Step 3: After removing the tick, clean the bite area and your hands with soap or rubbing alcohol.
Step 4: Never crush the tick with your hands, you can flush it down the toilet or dispose of it by putting it in rubbing alcohol.
For additional information about ticks, please visit the websites listed under references. If you have any questions about anything in this post, please contact the office at 610-675-1111. We are here to help and support all our nurses, aides, and caregivers. Our goal is to raise awareness to keep our healthcare professionals and patients safe.












